We don't live in a world of single chemicals. We never have. And yet, for most of the past century, that’s exactly how we’ve studied them.
Toxicology—the science of how chemicals affect our health—has long been a game of one-on-one: lead, mercury, tobacco smoke, DDT. Each chemical enters the ring alone, and we measure its punch. If the dose is high enough and the effect clear enough, it gets flagged as toxic. Case closed.
But in the real world, chemicals never act alone.
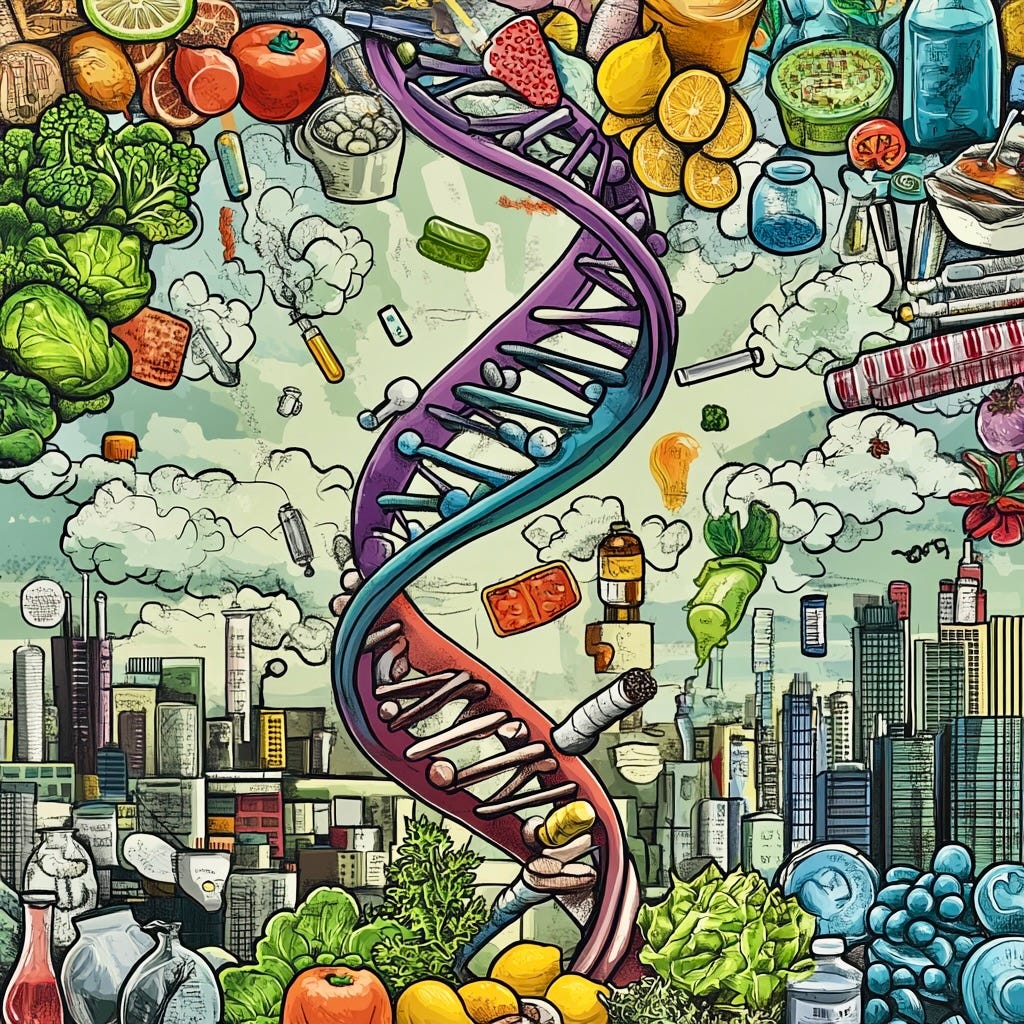
We are exposed to a complex, ever-changing cocktail of synthetic and natural compounds. They come at us in drips and traces—in our food, water, air, homes, and workplaces. They interact with each other, with our genes, with the nutrients we consume. They nudge development, tweak behavior, and sometimes, when the mix is wrong or the dose too high—they cause lasting harm.
We can see the consequences all around us: infertility, premature birth, childhood leukemia, asthma, autism, ADHD, heart disease, lung cancer, ALS—the list keeps growing.
That simple truth—that people are exposed to mixtures, not isolated substances—is what led to a quiet revolution in environmental health. The idea of studying chemical mixtures was born in a moment of humility. Scientists started asking: What if we’re missing the forest for the trees?
The Real-World Toxic Soup
In epidemiology, research from the 1970s to 1990s focused on one chemical at a time—lead, PCBs, or mercury—tracing their individual effects on child development. These first-generation studies were essential. They helped prove something that now seems obvious: early-life exposures to harmful substances can have lifelong consequences.
The second-generation studies, led by scientists like Frederica Perera, took a broader view—examining multiple pollutants at once, including air pollution, pesticides, and endocrine disruptors. These studies showed that it’s not just how much of a substance you are exposed to that matters—it’s also when you are exposed and what else you are exposed to at the same time.
The shift gained momentum as evidence piled up. Dozens of chemicals were detected in children even before birth. Researchers found that many toxic chemicals caused harm at extraordinarily low concentrations—far lower than regulators had assumed. Studies also revealed that some exposures didn’t just add up; they multiplied. Lead and tobacco smoke, for example, showed synergistic effects on ADHD—each doubling the risk on its own, but increasing it more than eight-fold when combined.
It was a profound insight: children aren’t exposed to just one chemical. They’re exposed to hundreds of chemicals—from the moment of conception to the end of life—and they’re exposed during critical windows of development.
When the Exposome Got a Name
It was a revolutionary shift in how we think about environmental risk—a counterweight to the genetic revolution. In 2005, British epidemiologist Christopher Wild gave it a name the "exposome", defined as the totality of environmental exposures over a lifetime. Think of it as everything non-genetic that influences your body—air pollution, stress, diet, and more. The concept took off. It offered a bold parallel to the genome—and it had a nice ring to it.
The exposome gave researchers a vocabulary to match reality. But it also carried a warning. Just as decoding the human genome didn’t deliver on its grandest promises, mapping the exposome was never going to be simple.
Francis Collins an American geneticist known for leading the Human Genome Project, declared in 2003, "The study of the genome will reveal over the next decade the hereditary factors that contribute to virtually all common diseases, including diabetes, cancer, heart disease, mental illness, and hypertension.
Instead, we learned that complexity resists quick fixes. The genome didn’t reveal a clear blueprint. It revealed a swamp of hidden interactions—with diet, stress, and yes, toxic chemicals.
Autism and the Spectrum of Interactions
Nowhere is this more evident than in our growing understanding of autism. We’ve discovered that prenatal exposures to certain chemicals, like pesticides and phthalates, may increase risk—but primarily in children who have specific genetic vulnerabilities or nutritional deficiencies.
Take folate, the B-vitamin essential for fetal brain development. Studies show that adequate maternal folate can help protect against autism, even in the presence of risk factors like air pollution or endocrine-disrupting chemicals. Others have shown that in utero exposure to BPA—which affects the enzyme aromatase—can alter brain development. Still others highlight how air pollution interacts with genetic susceptibility to increase risk.
Together, these studies reveal a basic truth: brain development lies on a spectrum, shaped by a symphony of influences—genetic coding, nutrient availability, and a shifting mix of environmental chemicals. Some exposures gently adjust the tune; others throw the whole system off-key. A symphony becomes a cacophony. The cumulative effect can alter a child’s developmental path in ways we’re only beginning to understand.
This shouldn’t be a surprise. We saw the same thing with lead. During the 20th century, widespread lead exposure didn’t just lower IQs; it altered behavior, contributed to impulsivity, and likely played a role in the rise of violent crime. When you expose a population to a powerful neurotoxin, you shift the curve. You don’t just harm a few; you change the norm.
Regulating One Chemical at a Time
Despite this growing evidence, our regulatory agencies still operate on a chemical-by-chemical basis. The U.S. EPA has reviewed fewer than 10% of the 80,000+ chemicals in commerce. At this pace, it would take centuries to evaluate them all, let alone understand how they behave in combination.
The idea of regulating chemical mixtures? That’s still science fiction.
It’s not that regulators are uninterested. It’s that the science—and the policy frameworks—haven’t caught up. Advances in statistical modeling are helping, but they’re still evolving. The questions are messy, and the funding limited. Moreover, to fully explore the exposome, we need large cohort studies.
The National Children’s Study That Wasn’t
For a moment, it looked like we might rise to the challenge. In the early 2000s, NIH launched the National Children’s Study, a ground-breaking effort designed to examine environmental influences on child health. It aimed to track 100,000 children from birth through adulthood.
In 2003, I attended an invitation-only workshop with Frederica Perera, Kári Stefánsson, Francis Collins, and a dozen NIH colleagues when Collins declared, “I will do nothing to jeopardize the National Children’s Study.” It sounded reassuring—until I thought about it. If I’d been a little savvier, I’d have known that when a high-ranking official feels the need to make that kind of promise out loud, the study is already in trouble.
And it was.
In 2014, Collins shut down the National Children’s Study after more than a decade of planning and a $1.3 billion investment. Officially, it was too ambitious and too expensive. Unofficially, it was political expediency—the chemical industry saw it as a threat, and Collins viewed it as competition for his own ambitious genetic study.
Like the former director of the study, I was convinced that Collins had personally engineered its demise. A once-in-a-generation opportunity to transform children’s health and lay the groundwork for what would become the exposome was lost.
And in the end, that loss—not decoding the human genome—may be Collin’s most enduring legacy.
What the Exposome Can—and Can’t—Do
The exposome holds tremendous promise. It may give us the tools to see the hidden connections between chemical mixtures, nutrition, and disease or disorders. It can reveal interactions like the one between low folate and high pesticide exposure, which sharply increases autism risk. Or the synergy between childhood lead exposure and in utero tobacco exposure, which raises ADHD risk by more than eight-fold when both are present—accounting for an estimated 31% of U.S. cases.
But we should be realistic about what the exposome can do. The complexity is staggering. Decoding the human genome was like mapping every road, alley, and sidewalk in a vast, unfamiliar city. Studying the exposome alongside it is like trying to predict traffic patterns in that city—hour by hour—for every resident, while accounting for weather, construction, detours, mood, and whether they skipped breakfast.
The answers won’t be simple. But we don’t need to wait for perfect science before we act.
We already know enough to regulate the worst offenders. We know that many chemicals are harmful even at very low levels. We know that children are uniquely vulnerable. And we know that the human body didn’t evolve to metabolize the thousands of synthetic chemicals we now carry in our bloodstreams, let alone the staggeringly high concentrations of toxic metals, like lead and arsenic.
Some of these chemicals—like thalidomide and DES—were drugs. Others are in plastics, pesticides, and other household products. But the effect is the same: whether they are prescribed or ingested along with heavily processed food or inhaled aircraft emissions, they have the potential to radically alter human evolution.
That should be enough.
So yes, let’s fund exposome research. Let’s push the science forward. But let’s also stop pretending we need more proof before we act.
The chemical soup is already upon us. The question is whether we have the courage to clean it up.



Great post, Bruce! For what it is worth, since 1958, Congress has required FDA and the food additive industry to consider the cumulative effect of chemically and biologically related substances in the diet, a major part of the cocktail. Not one by one. And not just additives but everything in the diet. FDA adopted rules in March 1959 explaining how that is to be done.
Coupled with the reasonable certainty of no harm standard, we have a safety standard that is stronger than EU's precautionary principle. At least in theory.
Unfortunately, the FDA and industry have ignored the requirement and its own rules. Dr. Maricel Maffini and I reviewed thousands of decisions and found no instances where FDA followed the law. We documented in study after study.
In September 2020, we and other public health advocates submitted a citizen petition demanding the agency fix the problem and that it start by telling industry they needed to address it - not ignore it. FDA has ignored that request too.
FDA's failure to consider cumulative effects is, I think, one of the root causes of the ultraprocessed food problem that is not coming to the forefront.
Tom Neltner